This newsletter is one of the most disturbing experiences I’ve had with a healthcare facility in relation to billing. It’s disturbing because I was already familiar with the ways healthcare facilities and insurance companies sometimes “game the system” to make profits. But I had never personally experienced such an egregious example of what appeared to be greed, until now. I’m not going to name the employees, including doctors, who I corresponded with during this experience, but I am going to share a string of correspondences that some of you may find shocking.
On April 1, 2021, I had blood work, which showed my prostate-specific enzyme (PSA) had risen to 20.5. PSA is a biomarker for all things prostate including prostate cancer activity. Mine should be zero since I no longer have a prostate after undergoing surgical removal followed by radiation. Despite a nice drop in my PSA after what was hoped to be definitive treatment, my PSA never got below 0.9 and has been steadily rising since. By this point, I had undergone numerous postoperative scans, none of which had shown evidence of cancer despite a rising PSA. I was feeling pretty blessed, but all of that was about to change.
On April 14, 2021, I underwent a positron emission tomography (PET) computed tomography (CT) scan at my radiation oncologist’s office called an Axumin scan. This scan is FDA approved for detecting prostate cancer, and a prior Axumin scan on June 12, 2018, just after my surgery, showed no evidence of cancer. I had also undergone a different type of PET scan called a prostate-specific membrane antigen (PSMA) PET scan on September 20, 2019, at UCLA Health in Los Angeles. It had also shown no evidence of cancer.
But because my PSA had continued to rise, and was now 20.5, the odds of a PET scan now showing cancer was very high. As I lay in the PET CT scanner in my radiation oncologist’s clinic on April 14, 2021, I wasn’t anxious. I was just feeling curious. I guess I had undergone so many of these types of scans that fear extinction had kicked in. Fear extinction is when a conditioned fear response lessens or resolves after being repeatedly exposed to the same fear-inducing situation. Because I had been in a similar situation so many times, and the results were always normal, I was no longer feeling fear in the scanner. That’s the theory anyway.
Once the scan was complete, Mike and I waited in an exam room for my radiation oncologist to review the results with us. Unfortunately, this time the scan was abnormal and showed a small area of activity in the area of my prostate bed where my prostate was prior to my surgery.
What’s even more unfortunate is that my radiation oncologist told us that he couldn’t radiate this area since the tissue had received the maximum radiation allowable. If he did radiate this area again, I would be at very high risk for complications including radiation proctitis, tissue breakdown, and fistula formation.
My doctor said that despite the PET scan lighting up in the prostate bed, he couldn’t see an actual tumor mass on the CT scan. He ordered a magnetic resonance imaging (MRI) scan, which is more sensitive for detecting a soft tissue mass such as a tumor. It also didn’t show anything, which suggested this was a very tiny tumor. I wasn’t having any symptoms from it and there was nothing to do except continue to monitor as I had already decided not to go back on androgen deprivation therapy (ADT). The goal of ADT is to lower testosterone, which is known to feed prostate cancer and make it grow.
I had made the decision to not go back on ADT for several reasons. Based on the fact the cancer had escaped the confines of my prostate and I had failed prostatectomy and radiation, I was considered incurable. Therefore, ADT would be palliative and only buy me some time. I had tried ADT, which made me miserable with hot flashes, night sweats, sleep deprivation, and severe depression.
But there was another option, and that was to have another PSMA PET scan. Now that the Axumin scan was abnormal and my PSA was even higher, the PSMA PET might light up. And if the PSMA lit up in the same area as the Axumin scan then the scans would be considered concordant, meaning they matched. Having concordant PET scans of different types is one criterion that some clinical trials use to determine eligibility for PSMA radioligand therapy. This is because concordant scans suggest that at least all of the radiographically visible tumors might be obliterated.
I’ve written about PSMA radioligand therapy in a prior newsletter, but I’ll do a quick recap since it’s a little complicated. PSMA is a protein found on most prostate cancer tumor cells, which if there, will light up on the PSMA PET scan. PSMA radioligand therapy involves injecting a radioisotope that latches on to the PSMA protein on the tumor cell surface and does a one-millimeter burst of radiation. This small burst of radiation kills the tumor cell and because the radiation field is so tiny, it does little collateral damage compared to regular radiation therapy.
PSMA radioligand therapy (RLT) does have side effects including nausea, dry mouth, and temporary bone marrow suppression, but overall, the side effects are well-tolerated and often temporary. PSMA RLT is also considered not curative, but in some studies, it induces a durable remission, meaning a long period without evidence of tumor activity. In Germany, some physicians are using PSMA RLT as a type of maintenance therapy whereby the patient returns for treatment each time the tumor activity recurs on a PSMA PET scan.
This is the main reason I wanted to do another PSMA PET scan. If concordant, I could potentially go to Germany for radioligand therapy. I contacted one of the companies that facilitate American prostate cancer patients going to Germany for radioligand therapy, and the company’s doctor ordered the PSMA PET scan. Any doctor can order the PSMA PET scan, but I wanted to be established with this company because they were well-connected with the clinic in Germany that accepts Americans for PSMA radioligand therapy.
Between the time I had gotten the first PSMA PET scan and now, the Food and Drug Administration (FDA) had granted approval for two academic teaching centers in the United States to use PSMA PET scanning with prostate cancer patients. The good thing about that FDA approval is that insurance companies would slowly but surely start to pay for this scan. The first time I underwent the PSMA PET scan at this facility, it was under the guise of a clinical study and I paid $2647.91 cash out of my own pocket. This is because it was not FDA approved at the time and no insurance company would pay for it.
I emailed UCLA Health about coming back for another PSMA PET scan and this was the response I received.
“Unfortunately FDA approval does not imply immediate reimbursement by Medicare or private insurances. Establishing routine insurance coverage will take at least several more months.
In the interim UCLA has adopted the following approach for offering PSMA scans as a clinical service:
Patients covered by Medicare
UCLA has set an out-of-pocket fee of $3300 for the 68Ga-PSMA-11 PET scan. Patients have to pay this amount on the day of the scan. UCLA will try to get at least partial reimbursement from Medicare, which would then be refunded to the patients. However, there is no guarantee that Medicare will provide any coverage.
Privately insured patients
We will try to obtain preauthorization for every patient.
Alternatively the referring physicians can attempt to obtain pre-authorization.
If preauthorization cannot be obtained, patients will have to pay $3300 on the day of the scan. Patients can then try to work directly with their insurances to get reimbursed.
We are well aware that these out-of-pocket costs pose a large financial burden on patients and we are working hard on getting full CMS and private insurance coverage.”
Great! They would accept me for another scan as long as I had a referring physician, which I did. The facility also informed me that there was a two-month wait to be seen. I wasn’t surprised at the wait time given that only two facilities in the U.S. had been approved to do it.
I booked my flight and made hotel reservations. My plan was to fly in two days before the scan, just to be on the safe side, since so many flights were being canceled because of the pandemic. Then I would take a red-eye flight back the night of the scan. I asked my sister Dianne to join me for support. We met at the airport and took a car to the hotel. On the bright side, I got to make a mini-vacation out of this with my favorite sibling.
On the morning of June 25, 2021, we walked to the imaging center and I checked in. The receptionist told me that I wouldn’t have to pay cash because my health insurance company had agreed to cover the scan. That was a nice surprise. I underwent the PSMA PET CT scan, which included drinking a liter of red fluid and getting an intravenous injection of the radioisotope.
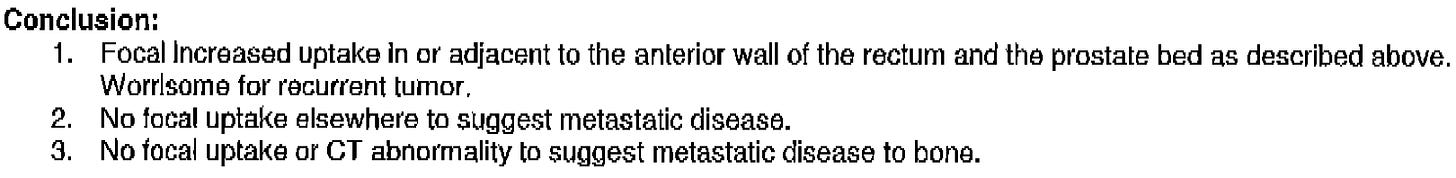
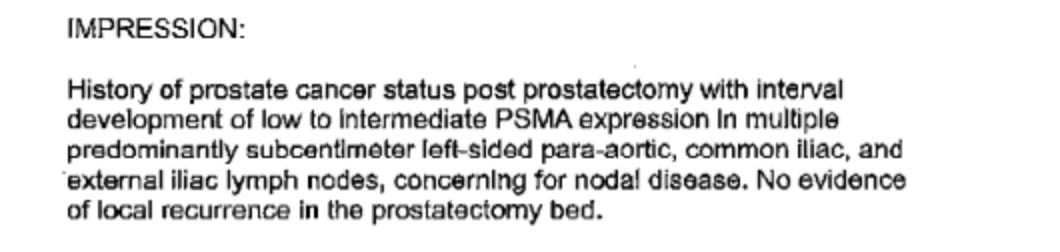
I returned home and on July 1, 2021, I received a fax with the report of the PSMA PET scan. This was its conclusion:
So, there were two concerning issues here. One was that it showed multiple small tumor deposits in my left-sided lymph nodes starting in my pelvis and rising to the lower part of the left side of my aorta. All of these deposits were 4mm in size. I wasn’t surprised given that the PSMA PET scan is more sensitive for detecting metastases than any other PET scan for prostate cancer. So this might be why the lymph node metastases didn’t show up on the Axumin PET scan two months earlier.
The other concerning finding was that the tumor tissue that had lit up in the prostate bed on the Axumin scan two months earlier wasn’t expressing the prostate-specific membrane antigen (PSMA) protein. This meant the scans weren’t concordant, meaning they weren’t a match.
I wouldn’t be eligible for PSMA radioligand (RLT) therapy in Germany because the radioligand therapy wouldn’t radiate the tumor in the prostate bed. The RLT would only radiate the tiny left-sided lymph node metastases. Not only that, studies show that for PSMA RLT to be most effective, the PSMA PET scan should show high uptake of the radioisotope. Mine only showed low to intermediate uptake. It would not be worth going to Germany and paying $20,000 for the treatment because I wasn’t a candidate for a good response.
I accepted this fact and remain determined to find a way to cure this thing.
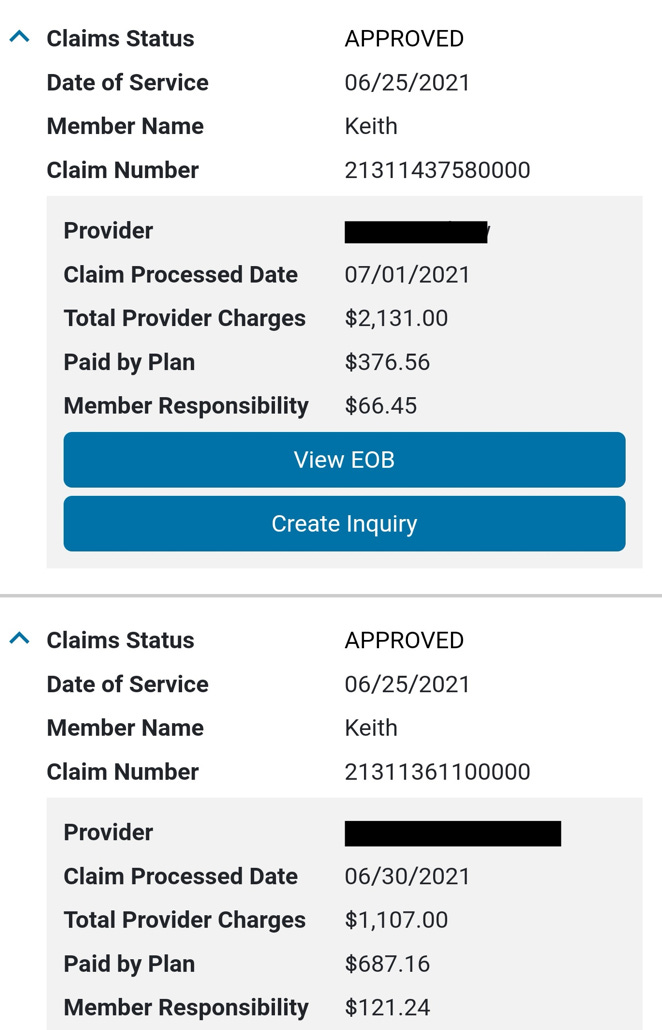
Then a few days later, I received an email from my health insurance company that new information was available in my account. I signed in and found this:
This hospital somehow justified charging my insurance company $19,266.63 for a PET scan. In addition, I found this:
So even though I never saw a physician at the time of my PSMA PET scan, UCLA Health charged my insurance company a total of $3238.00 in physician charges in addition to the $19,266.63 for a grand total of $22,504.63. I’m assuming one of the physicians was the radiologist who read the scan and the other physician was supervising the technician who injected the radioisotope.
So despite only charging cash-pay patients $3300.00, this facility somehow justified charging my insurance company $22,504.63.
Does this seem right to you?
It didn’t to me, so I promptly looked up the email addresses of the two physicians overseeing this PSMA PET department and emailed them. I did not let them know I was a physician because I wasn’t interested in professional courtesy, but was interested in seeing how they justified these outrageous charges. I did not correct any misspellings in the emails so as not to alter them. This is what I wrote:
Dear Dr. [Name]
I recently underwent PSMA PET imaging at your facility and wanted to express my concerns about how your department portrays its billing and the actual billing experience I had. I understand that UCLA and UCSF are the only two imaging centers in the United State to receive FDA approval for PSMA PET scanning. This is a great honor, but with great honor comes a great responsibility to patients.
This is especially true given that many of the men who will receive this specialized type of PET scan have advanced prostate cancer, which you know is incurable. The majority of these men have undergone multiple procedures, are ravaged by disease, have been told they are incurable, and many also have additional stress related to the financial burden this disease has placed on them and their families.
I have already tried to resolve this billing issue by reaching out to your patient advocate, who in turn presented this to your billing department. Your billing department's response was for me to pay up!
On May 5, 2021, I received an email (see attached) from [Name] notifying me that if preauthorization of the PSMA PET scan could not be obtained through my insurance, that my out-of-pocket cost would be $3300.00. She also said, "We are well aware that these out-of-pocket costs pose a large financial burden on patients and we are working hard on getting full CMS and private insurance coverage."
I missed three days of work, flew across the country, and stayed two nights in a hotel to have this test. On June 25, 2021, I showed up for the scan and was told by the very nice gentleman at the desk that I owed no money, and that my insurance was covering the test.
I returned to my home in Florida and was notified by my insurance company that Blue Cross Blue Shield (BCBS) was billed a total of $22,504 for this PET scan. BCBS paid your facility and its doctors $12,148.93.
I was informed that your facility would be billing me $2143.89 in addition to the $12,148.93 you had already received from BCBS, for a grand total of $14,292.82 net payment to your facility. This is a shocking 23% markup over the original cash price quote of $3300.00.
Dr. Michael Hofman, Australia's leading expert on PSMA theranostics, said in a www.urotoday.com article that PSMA PET scans cost approximately $800.00 (US).
[Name’s] statement, "We are well aware that these out-of-pocket costs pose a large financial burden on patients and we are working hard on getting full CMS and private insurance coverage" is not reflected in your billing procedures.
Why would UCLA charge me an additional $2143.89 over the $12,148.93 my insurance company already paid you if UCLA was truly concerned about the large financial burden on patients? I have metastatic prostate cancer and have multiple medical bills like this.
So if you are not covered by insurance, the total bill is $3300.00, but if you're covered by insurance, the total bill is $22,504.00. That makes no sense and is a perfect example of why healthcare billing in the United States is viewed as a type of gaming of the system - billing insurance companies extravagant amounts in an attempt to get high returns. In addition, thousands of patients a year are forced into bankruptcy because of health-related bills.
Why is it that UCLA would have been fine with billing me only $3300.00 if my insurance wouldn't participate, but then bills a grand total of $22,504.00 when my insurance agrees to participate? This has an appearance of greed. It also has an appearance that your facility's billing procedures appear to be using insurance-covered patients to subsidize the fees for patients that aren't covered by insurance for this test. That seems unethical.
I'm asking that UCLA and its doctors accept the $12,148.93 BCBS paid, as payment in full, and not bill me the additional $2143.89. If UCLA is truly concerned about the financial burden on patients, then it seems like your facility would agree to this.
Thanks for taking the time to read this email and I look forward to hearing back from you.
Sincerely,
Keith Holden
I’ll admit that I’m financially blessed to be able to pay my insurance co-pay amounts, but the appearance of greed and using insurance-covered patients to subsidize cash-payors rubbed me the wrong way. I’ll also admit to acting like a drama queen here, but I was genuinely interested in how they were going to try and justify this type of egregious billing practice.
Surprisingly I heard back from both program directors, and what was even more surprising was how they both seemed shocked and appalled by the billing practice of their own facility. I realized both physicians genuinely care about their patients and actually took the time to attempt to help out a concerned patient. Kudos to both of them!
Here is the response from one of the physicians:
Dear Mr. Holden,
We will be in touch on Monday to resolve this issue. We do apologize for causing stress and axiety. This is clearly a mistake!
Sincerely,[Name]
The other department director also kindly responded:
Hello Keith,
First, I would like to apologize in the name of [Name] for your situation.
This is a terrible nonsensical system.
I'm [nationality] (very different healthcare system there) and I m really astonished by such stories.
I'm still learning but I just really hate it.
Please do not pay anything.
We will fix this.Info was brought to the team.
Thanks a lot for your detailed email, very helpful.
Again, so sorry for this
Best regards,
[Name]
The following day, I received a phone call from this facility with two women on the call at the same time. One woman was a practice manager for the department and the other woman was associated with, guess which department - the billing department. I was very patient and kind during this phone call but felt attacked as if I had threatened not to pay them a dime. Neither one wanted to let me get a word in, and when one paused, the other jumped in.
These women could have cared less if I had cancer or if I could or couldn’t afford to pay my portion of the bill. They both seemed quite upset that I had actually corresponded with the two physician directors in the imaging department. I put them on speakerphone so my husband could hear what they were saying. One word described the look on his face - horrified!
About five minutes into the conversation, the call was miraculously disconnected. I say miraculously because I was starting to feel ill by the way they were speaking to me. They tried to call back and I didn’t answer the phone.
I then emailed both program physicians about my experience with these two women:
Hi [Dr. Names],
I just had a very disturbing conversation with two women from the imaging center. I believe one was named [Name] and the other [Name]. They were double teaming me by one jumping in if the other one didn't make a clear point, but neither of them was letting me express the points I relayed to both of you in the email.
They said neither of you understood my email correctly, which I find hard to believe because it was written very succently and in explicit detail.
They were very rude, speaking loudly and over me, and talking down to me. They would not even entertain the concepts I pointed out in the email, which you both seemed to understand. All they wanted to discuss was the fact I owed UCLA money based on my insurance plan.
I can't tell you how frustrating their phone call was. I wish I had thought to record it so you could hear how rude they were. I really would have expected better communication from a facility like UCLA.
It seemed like [Dr. Name] understood the points I was making so I was quite relieved, until I received their phone call today.
I'll call the billing department tomorrow to try and set up some kind of payment plan.
Thanks for listening and trying to intervene on my part.
My best wishes to both of you and your program.
Sincerely,
Keith Holden
And the physicians both kindly responded. Here is the first email response:
Hi Keith
I believe I talked too quickly.
Again, like I said I’m still learning this crazy nonsensical system.
These numbers ($22000, $15000, $12000 etc …) are completely disconnected form the reality and the value of the actual procedure.
These are created to align on insurances policies, hospital charges etc..
A market where the numbers have no correlation with the value.
I learn that charge is different than cost than different value...
Unfortunately I have no (realistic) idea on how to fight this craziness.
This is not UCLA only, the whole US healthcare system works like that in a vicious circle of inflation.
In your case,
You can be out of the system, without insurance by paying the out-of-pocket cost of 3300 USD.
3330 USD is expensive but represents decently what it actually costs (especially in comparison to 22K or 12K).
If you use your insurance, then you play THEIR Game. With their numbers. With charges and costs negotiated on a market rule.
You just have ignore the 22K, 15K, 12K you see on a bill that are completely artificial.
Bubble money.
At the end you would need to pay 2140 USD, considered as your-co-pay.
It is still expensive but 1000 less that the non-covered price of the scan…
That is all I was able to get.
Sorry again
[Dr. Name]
This physician even attached a PowerPoint slide from his facility that explained why you have to “game” the insurance companies to get better reimbursement. I found it hilarious that he would do that.
I’m not going to include it in this newsletter because I have a feeling it would be too embarrassing to their facility. I’m going to use some similar dollar numbers to describe what was on the slide but only a few dollars off.
It gave an example of a surgical procedure and then gave a breakdown of “average hospital charge to insurance” - $88,099.99, “commercial insurer payment to hospital” - $25,545.00, and “average hospital input cost” - $10,665.00.
The slide concluded by saying that hospitals rely on payments from commercial insurers, which tend to be above hospital input costs to balance out payments from public payers like Medicaid and Medicare, which tend to be below hospital costs and - bottom line - unprofitable.
So I guess in regards to PSMA PET scanning in this facility, cash payers are like Medicare and Medicaid payers. And those of us who have commercial health insurance plans that agree to pay a portion of the facility’s knowingly inflated price, are subsidizing these cash payers just like commercial insurance payments subsidize Medicaid and Medicare payers. Why subsidize? As the slide said, for profit! This sums up a big part of what is wrong with medicine in the United States.
The other physician kindly then responded:
Dear Mr. Holden,
[Name] mail hopefully clarified the issue a little better.
Pleaae wait with the payment plan until we have a chance to talk.
Sincerely,
[Name]
I never did get a chance to speak with either physician. I knew I had already taken up enough of their time. In addition, I realized that they were both probably as disgusted as I was with the way these inflated billing practices work.
The average salary for the top three executives of this facility in 2020 was 1.2 million dollars, including bonuses. It was reported that in 2016 the CEO of this facility had his annual salary doubled amidst budget cuts and tuition hikes.
Here’s an idea:
You and other major health centers should stop giving exorbitant pay raises to your highly paid senior executives and use that money to lobby members of Congress to increase Medicaid and Medicare payouts so you can stop overinflating charges for services and procedures. This should disincentivize commercial insurance companies to stop overpaying for services and procedures. In turn, patient co-pays can be reduced to more fair prices.
To understand how major commercial insurance companies are complicit in this healthcare billing debacle, read this very interesting article.
I’ll be in touch soon with my next update.
Keith R. Holden, M.D.





I experienced this but to a lesser degree. My pulmonologist told his office to stop billing me copays. It was a nice gesture.
Very Sad State of Affairs in the American Healthcare System. I am sorry that you had to experience this which only compounds the stress of having prostate cancer.